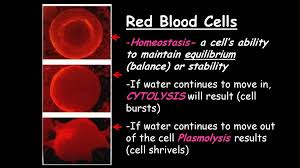
What causes red blood cells to burst cytolysis?
This means the water wants to move into the cell to even things out. It’s like a party where everyone wants to get inside a crowded room. The cell, trying to accommodate all this incoming water, swells up like a balloon being blown up. But there’s a limit! The cell membrane can only stretch so much before it can’t handle the pressure anymore and pops, causing cytolysis.
This bursting happens because the cell membrane is a delicate structure that can’t withstand the force of the water rushing in. It’s like a balloon stretched too far, eventually reaching a point where it can no longer hold the air and bursts.
Think of it this way:
Hypotonic solution: Water outside the cell is more abundant than inside the cell.
Water movement: Water flows from the area of high concentration (outside) to the area of low concentration (inside).
Cell swelling: The cell absorbs water, leading to swelling.
Cytolysis: The cell membrane can only stretch so much, and eventually bursts due to the pressure from the inflowing water.
So, hypotonic solutions are the culprits behind red blood cell cytolysis. It’s a natural process that happens when there’s an imbalance in water concentration, and the cell struggles to keep up with the influx.
What happens when a red blood cell bursts?
Hemolytic anemia occurs when your body destroys red blood cells faster than it can replace them. There are two main types of hemolytic anemia:
Inherited hemolytic anemia is caused by a genetic defect that makes red blood cells fragile and more likely to burst.
Acquired hemolytic anemia is caused by factors such as infections, autoimmune disorders, or certain medications.
What happens when a red blood cell bursts?
Think of a red blood cell as a tiny, flexible, doughnut-shaped package carrying oxygen around your body. Inside that package is hemoglobin, a protein that loves to hold onto oxygen molecules. When a red blood cell bursts, it’s like the package spills its contents. The hemoglobin gets released into the bloodstream, and this can cause a few things to happen:
Reduced oxygen carrying capacity: Fewer red blood cells mean your body has less capacity to carry oxygen, leading to a condition called anemia. This can make you feel tired and weak.
Spleen overload: Your spleen is a hardworking organ that filters your blood, and it also helps to remove old and damaged red blood cells. When red blood cells burst frequently, your spleen gets overwhelmed trying to clear the mess. This can make your spleen larger and more prone to infection.
Kidney issues: Your kidneys help regulate the amount of fluid and waste products in your body. When a lot of hemoglobin gets released from burst red blood cells, it can strain your kidneys. This can lead to kidney problems in severe cases.
It’s important to remember that hemolytic anemia can range from mild to severe. If you’re experiencing symptoms like fatigue, shortness of breath, or jaundice, it’s important to talk to your doctor to rule out any underlying medical conditions. They can help diagnose the cause of your anemia and recommend the best treatment plan for you.
What is it called when blood cells explode?
Think of red blood cells as tiny delivery trucks, carrying oxygen throughout your body. When these cells break down, it’s like the trucks spilling their cargo. This can happen for a variety of reasons, and it’s not always a cause for alarm. Sometimes, it’s a natural process, like when old red blood cells are recycled by your body. However, other times it can be a sign of a serious medical condition.
Here’s the thing: When red blood cells break down, they release their contents into the surrounding fluid. This includes hemoglobin, a protein that gives blood its red color and is essential for carrying oxygen. If a lot of red blood cells break down, the hemoglobin can build up in your blood, leading to complications.
There are a few different ways that hemolysis can occur:
Intravascular hemolysis happens when red blood cells break down inside blood vessels. This can be caused by things like infections, certain medications, or autoimmune disorders.
Extravascular hemolysis happens when red blood cells are destroyed outside of blood vessels, usually in the spleen. This is often a normal process as part of the body’s natural recycling of old red blood cells.
Hemolysis can be a serious medical condition if it’s happening too quickly or if it’s caused by an underlying health problem. If you have any concerns about hemolysis, you should talk to your doctor. They can help you determine the cause of the hemolysis and recommend the best course of treatment.
What happens during cytolysis?
Water naturally moves from areas of high concentration to areas of low concentration, seeking to balance things out. In this case, water rushes into the cell through the cell membrane, attempting to dilute the higher concentration of substances inside. This influx of water puts pressure on the cell membrane, eventually causing it to rupture, leading to cell death.
Imagine a balloon filled with a concentrated sugary solution. If you place it in a bowl of pure water, the water will try to enter the balloon to dilute the sugary solution. As more water enters, the balloon will expand and eventually burst. This is similar to what happens during cytolysis.
However, not all cells are equally susceptible to cytolysis. Some cells have mechanisms to prevent excessive water entry, such as osmoregulatory proteins that pump out excess water or specialized aquaporins that regulate water flow across the membrane. These mechanisms help cells maintain their internal balance and prevent them from bursting.
The process of cytolysis is important for various biological processes, including:
Immune response: Immune cells like cytotoxic T cells use cytolysis to kill infected or cancerous cells by releasing substances that induce osmotic lysis.
Pathogenesis: Some bacteria use toxins that cause cytolysis of host cells, contributing to their virulence.
Understanding cytolysis is crucial for comprehending various biological processes and developing strategies for treating diseases or designing new drugs.
What condition causes red blood cells to burst?
Think of red blood cells as tiny delivery trucks carrying oxygen throughout your body. In hemolytic anemia, these trucks are getting damaged and destroyed prematurely. This can happen for various reasons, and it leads to a shortage of healthy red blood cells, causing symptoms like fatigue, weakness, and shortness of breath.
What causes red blood cells to burst?
There are many reasons why red blood cells might burst. Some common causes include:
Inherited disorders: These are genetic conditions passed down from parents, affecting the structure or function of red blood cells. Examples include sickle cell anemia and thalassemia, where the shape or hemoglobin content of red blood cells is altered, making them fragile and prone to breaking.
Autoimmune diseases: In these conditions, the body’s immune system mistakenly attacks and destroys its own red blood cells. Autoimmune hemolytic anemia is one such disorder.
Infections: Some infections, like malaria, can cause red blood cells to burst as the parasite replicates inside them.
Medications: Certain drugs can trigger hemolysis in susceptible individuals.
Chemical exposure: Exposure to toxins like lead or arsenic can also damage red blood cells.
The specific cause of hemolysis needs to be diagnosed by a doctor through blood tests and other examinations. Early diagnosis and appropriate treatment are crucial for managing hemolytic anemia and improving the quality of life for those affected.
What causes red blood cells to pop?
Imagine your red blood cells as tiny, flexible balloons. They’re designed to squeeze through narrow blood vessels and deliver oxygen to every part of your body. But sometimes, things happen that make these balloons fragile and prone to popping.
For example, some people inherit genetic conditions that make their red blood cells abnormally shaped or more fragile. These cells are like balloons with thin walls or uneven shapes. They’re more likely to break apart as they travel through your bloodstream.
Other times, infections can cause your immune system to attack your own red blood cells. It’s like your body accidentally mistakes its own red blood cells for invaders, causing them to burst. Some medications can also trigger a similar reaction, making your red blood cells more vulnerable.
When your red blood cells break down, you lose oxygen-carrying capacity in your blood. This can lead to various symptoms, including fatigue, shortness of breath, and paleness. It’s like having fewer balloons to carry oxygen to your muscles and organs.
Fortunately, there are treatments for hemolytic anemia, including medications to suppress your immune system, blood transfusions, and sometimes even bone marrow transplants. These treatments help your body produce healthy, durable red blood cells, allowing your body to function properly.
What can cause red blood cells to burst during collection?
If you’re collecting blood for a test that requires a full tube (like a prothrombin time test), and a partial draw isn’t acceptable, you can always ask for a smaller tube. This way, you can reduce the pressure on the blood and minimize the risk of cell rupture.
It’s also important to be aware of hematomas. A hematoma is a collection of blood outside of a blood vessel. If you collect blood from a hematoma, the blood can be contaminated with cells that have already broken down, leading to inaccurate results. Always avoid collecting blood from a hematoma.
A Little More About Red Blood Cells and Vacuum Tubes
Think of red blood cells as tiny, fragile balloons carrying oxygen throughout your body. Just like a balloon, they can burst if they’re squeezed or stretched too quickly. The vacuum inside a blood collection tube is like a big suction that draws the blood in. If the vacuum is too strong, it can cause the red blood cells to rupture.
Here’s a simple analogy: Imagine you’re filling a balloon with air. If you blow into it gently, the balloon will inflate without bursting. But if you blow hard and fast, the balloon might pop. It’s the same with red blood cells!
Some blood collection tubes have a lower vacuum, which helps to reduce the force with which the blood enters the tube. If you’re concerned about red blood cells bursting, you can always ask your healthcare provider to use a tube with a lower vacuum.
You can also minimize the risk of cell rupture by using the right size tube for the amount of blood being collected. If the tube is too small, the blood will be forced into a smaller space, increasing the pressure and the risk of cell rupture. On the other hand, if the tube is too large, you might not collect enough blood for your test. It’s always a good idea to use the appropriate size tube for the amount of blood being collected.
Ultimately, the goal is to collect blood as gently as possible, minimizing the chance of red blood cells bursting. If you have any questions or concerns, don’t hesitate to talk to your healthcare provider or phlebotomist!
How do you stop red blood cells from bursting?
It’s important to note that removing the spleen is usually considered when other treatments, such as corticosteroids or immunosuppressants, haven’t been successful in controlling the destruction of red blood cells. Corticosteroids are medications that help reduce inflammation, and immunosuppressants help suppress the immune system.
The spleen plays a crucial role in the body’s immune system, filtering out bacteria and other harmful substances from the blood. However, in cases of severe immune hemolysis, the spleen can become overactive and destroy red blood cells at a faster rate than normal. Removing the spleen can help to reduce the rate of red blood cell destruction and prevent complications like anemia.
After a splenectomy, individuals are more susceptible to infections, and lifelong antibiotic therapy is often recommended. This is because the spleen plays a significant role in fighting infection, and its absence can make the body more vulnerable to certain bacteria, particularly encapsulated bacteria.
Why does a red blood cell burst in hypertonic?
Think of it like this: Imagine a balloon filled with water. If you put the balloon in a very salty solution, the water inside the balloon will try to move out to dilute the saltiness of the solution. This is because nature always tries to balance things out.
Similarly, the water inside the red blood cell will try to move out into the hypertonic solution to balance the concentration. This movement of water out of the cell causes the cell to shrink and become wrinkled, like a raisin.
While the red blood cell might shrink in a hypertonic solution, it doesn’t burst. Instead, it undergoes crenation, which is a process of shrinking and becoming wrinkled. This is because the cell membrane is strong enough to withstand the pressure changes caused by the water moving out of the cell. However, if the concentration difference between the inside and outside of the cell is too great, the cell might be damaged or even destroyed.
In conclusion, red blood cells placed in a hypertonic solution don’t burst, they shrink and become wrinkled. This process is called crenation and is a natural response to the concentration differences between the inside and outside of the cell. The cell membrane is strong enough to handle the pressure changes, but if the difference is too great, the cell might be damaged.
See more here: What Happens When A Red Blood Cell Bursts? | Red Blood Cell Bursts Cytolysis
What causes cytolysis?
Think of it like a balloon. If you keep adding air, eventually the balloon will burst. Similarly, if a cell is placed in a hypotonic environment, it will take in too much water and burst. This is why it’s important for cells to maintain a balance of water and solutes.
Another factor that can contribute to cytolysis is the activity of other cells. For example, some cells produce cytolytic enzymes that can break down the cell membrane. These enzymes are often produced by immune cells to target and destroy infected or cancerous cells. Additionally, mechanical damage to the cell membrane, such as from a physical injury, can also cause cytolysis.
Let’s take a closer look at how tonicity plays a role in cytolysis. Cells are surrounded by a membrane that acts as a barrier between the inside and outside of the cell. This membrane is selectively permeable, meaning that it allows some substances to pass through while blocking others. Water is one of the substances that can pass through the cell membrane easily.
When a cell is placed in a hypotonic solution, the concentration of water outside the cell is higher than inside the cell. This creates a concentration gradient, causing water to move from the area of higher concentration (outside the cell) to the area of lower concentration (inside the cell). This influx of water causes the cell to swell, putting pressure on the cell membrane. Eventually, the pressure becomes too great, and the cell membrane ruptures, leading to cytolysis.
Cytolysis is a natural process that plays an important role in the body’s defense mechanisms. However, it can also be a harmful process, particularly if it affects healthy cells. Understanding the factors that contribute to cytolysis is essential for understanding how cells function and how to protect them from damage.
What are examples of cytolysis?
One common example of cytolysis is hemolysis, which is the breakdown of red blood cells. This can happen when red blood cells are exposed to certain toxins, such as those found in snake venom. Hemolysis can also occur if red blood cells are placed in a solution that is too salty or too dilute. In these cases, the water will either move out of or into the red blood cells, causing them to shrink or swell, respectively. This change in volume can cause the cell membrane to rupture, leading to hemolysis.
Another example of cytolysis is osmotic lysis, which is the bursting of cells due to changes in osmotic pressure. Osmotic pressure is the pressure that needs to be applied to a solution to prevent the inward flow of water across a semipermeable membrane. When cells are placed in a solution with a lower osmotic pressure than the inside of the cell, water will flow into the cell, causing it to swell. If the cell swells too much, it can burst, leading to osmotic lysis.
These are just a couple of examples of cytolysis. There are many other ways that cells can be destroyed, and cytolysis is a process that is involved in a variety of biological processes.
Understanding Cytolysis and its causes can help us better understand how cells function and how they can be damaged. For example, hemolysis is a major concern in blood transfusions, as mismatched blood types can lead to the destruction of red blood cells. Osmotic lysis is also a factor in some diseases, such as sickle cell anemia, where red blood cells are abnormally shaped and more susceptible to lysis. By understanding the mechanisms of cytolysis, we can develop strategies to prevent cell damage and treat related diseases.
What causes a blood cell to burst in a hypotonic solution?
Since water naturally moves from areas of high concentration to areas of low concentration, water rushes into the red blood cell. This influx of water causes the cell to swell and eventually burst, a process called cytolysis or osmotic lysis.
Think of it like this: Imagine a balloon filled with air. If you put that balloon in a room with a lot of air, nothing much happens. But if you put that same balloon in a vacuum chamber, the air from inside the balloon will rush out, causing the balloon to collapse.
That’s essentially what happens to a red blood cell in a hypotonic solution. The pressure from the water entering the cell eventually becomes too much, causing the cell membrane to rupture.
But don’t worry, this is a controlled process. Our bodies have ways to regulate the movement of water in and out of cells to prevent this from happening too often.
What does cytolysis mean?
Think of a balloon. If you keep adding air, it will eventually burst. Similarly, when a cell absorbs too much water, it can’t hold it all and eventually explodes. This process, also known as osmotic lysis, is a common occurrence in biology. It plays a vital role in various processes like:
Immune Response: Cytolysis is a key mechanism in our immune system’s fight against harmful bacteria and viruses. Immune cells like cytotoxic T lymphocytes (CTLs) use cytolysis to destroy infected cells.
Drug Delivery: Scientists are developing new drugs that utilize cytolysis to target and destroy specific cells, like cancer cells. These drugs are designed to trigger cytolysis in the target cells, leaving healthy cells unharmed.
Cell Culture: In laboratory settings, scientists use cytolysis to study cell function and develop new drugs. By carefully controlling the environment, they can induce cytolysis and observe how cells react to different stimuli.
Understanding cytolysis is crucial for comprehending various biological processes. It helps us understand how cells function, how our immune system works, and how diseases develop. By studying cytolysis, we can develop new therapies and treatments for various health conditions.
See more new information: linksofstrathaven.com
Red Blood Cell Bursts: Understanding Cytolysis
Let’s start with the basics. Red blood cells, or erythrocytes, are these tiny little cells that are responsible for carrying oxygen throughout your body. They’re shaped like little donuts, but without the hole in the middle. They’re packed full of hemoglobin, a protein that binds to oxygen and then releases it into your tissues.
Now, cytolysis is the process where a cell bursts, and in the case of red blood cells, it can be a pretty serious problem. Think of a balloon that’s filled with water and then gets poked. The water spills out, right? The same thing happens with red blood cells – they get damaged, and their contents leak out.
What causes red blood cells to burst?
Well, there are a bunch of different things that can trigger cytolysis.
Hypotonic solutions are one big culprit. These are solutions where the concentration of water is higher outside of the cell than it is inside. Think of it this way: water always wants to move from an area where there’s a lot of it to an area where there’s less. So, when red blood cells are in a hypotonic solution, water rushes into the cell to try to even things out. This causes the cell to swell up like a balloon that’s been over-inflated, and eventually, it bursts.
Certain toxins can also cause cytolysis. These toxins can damage the cell membrane, which is like the skin of the cell, and make it more permeable to water. This allows water to flow in, causing the cell to swell and burst.
Mechanical stress can cause cytolysis too. Think about a red blood cell being squeezed through a tiny blood vessel. If the vessel is too narrow, the cell can get damaged and burst.
Diseases, like sickle cell anemia, can also lead to cytolysis. This is because the red blood cells in sickle cell anemia are shaped like crescent moons instead of donuts. This makes them more fragile and prone to bursting.
What happens when red blood cells burst?
Well, that’s not good news. Here’s what happens:
Oxygen transport is disrupted. When red blood cells burst, the hemoglobin leaks out, and it can no longer carry oxygen. This means that your tissues don’t get the oxygen they need, and this can lead to problems like tissue damage and organ failure.
Immune response. The body’s immune system kicks in to clear out the debris from the burst red blood cells. This process can cause inflammation and other problems.
Anemia. When red blood cells burst, you lose blood cells, and this can lead to anemia, a condition where you don’t have enough red blood cells to carry oxygen around your body.
Jaundice. When red blood cells break down, they release a yellow pigment called bilirubin. If your body can’t get rid of bilirubin quickly enough, it can build up in your blood and tissues, making your skin and eyes look yellow – this is called jaundice.
How to prevent red blood cell bursts
Now, that’s the bad news, but there are some things you can do to help prevent cytolysis:
Stay hydrated. This is especially important if you are doing any strenuous activities. Water helps to keep your blood volume up and prevents your red blood cells from getting too crowded in the blood vessels.
Eat a healthy diet. Make sure you’re getting enough iron in your diet. Iron is essential for the production of hemoglobin, the protein that carries oxygen in red blood cells.
Avoid toxins. Stay away from things that can damage your red blood cells, like certain chemicals and pollutants.
Treat underlying conditions. If you have a condition that can cause cytolysis, like sickle cell anemia, make sure you are getting the proper treatment.
The Takeaway
Red blood cell bursts or cytolysis can have serious consequences, so it’s important to understand what causes them and how to prevent them. By taking care of yourself and avoiding harmful things, you can help to keep your red blood cells healthy and strong.
FAQs
Q: What are some other names for red blood cell bursts?
A: Besides cytolysis, hemolysis, and erythrocyte lysis are also commonly used to describe the bursting of red blood cells.
Q: Can red blood cell bursts be reversed?
A: Unfortunately, once a red blood cell bursts, it can’t be put back together. However, your body can produce new red blood cells to replace the ones that have been lost.
Q: Can red blood cell bursts be detected?
A: Yes. There are several tests that can detect hemolysis, such as a complete blood count (CBC) or a reticulocyte count.
Q: What are some of the symptoms of red blood cell bursts?
A: The symptoms of hemolysis can vary depending on the severity of the condition. However, some common symptoms include fatigue, shortness of breath, pale skin, and jaundice.
Q: How serious are red blood cell bursts?
A: The seriousness of hemolysis depends on the cause and the severity of the condition. In some cases, it can be a minor problem that resolves on its own. In other cases, it can be life-threatening.
Q: Is there a cure for red blood cell bursts?
A: There is no cure for hemolysis, but the underlying cause can often be treated, which may help to prevent further hemolysis.
Q: Can red blood cell bursts be prevented?
A: While not all hemolysis can be prevented, you can take steps to lower your risk. These include staying hydrated, eating a healthy diet, avoiding toxins, and getting regular medical checkups.
I hope this information has been helpful. If you have any more questions about red blood cell bursts or cytolysis, please don’t hesitate to ask.
Cytolysis – Process with Definition, Meaning, & Importance
If cells are placed in pure water, a massive influx of water occurs, which causes the cell to burst. A 100 ml saline solution with 0.9 grams of NaCl (sodium Science Facts
Cytolysis – Biology Simple
Cytolysis refers to the rupture or destruction of cells. Examples of cytolysis include hemolysis, where red blood cells break apart, and osmotic lysis, biologysimple.com
Tonicity: hypertonic, isotonic & hypotonic solutions (article) | Khan …
If placed in a hypotonic solution, a red blood cell will bloat up and may explode, while in a hypertonic solution, it will shrivel—making the cytoplasm dense and its contents Khan Academy
Measuring osmosis and hemolysis of red blood cells
By placing red blood cells in solutions of differing osmolarities and tonicities, this experiment demonstrates the effects of osmosis and the resultant changes in cell volume. American Physiological Society Journal
Physiology, Osmosis – StatPearls – NCBI Bookshelf
When placing a red blood cell in any hypertonic solution, there will be a movement of free water out of the cell and into the solution. This movement occurs through osmosis because the cell has more free National Center for Biotechnology Information
Red Blood Cell Metabolism In Vivo and In Vitro – PMC
Red blood cells (RBC) are the most abundant cell in the human body, with a central role in oxygen transport and its delivery to tissues. However, omics technologies National Center for Biotechnology Information
A Comprehensive Review of Our Current Understanding of Red
Introduction. The blood of mammals, such as humans, as well as of birds, reptiles, and teleosts, contains red blood cells (erythrocytes). Human red blood cells, National Center for Biotechnology Information
Cytolysis – an overview | ScienceDirect Topics
In certain infections antibodies are formed against host erythrocytes and these cells are particularly sensitive to lysis. The haemolysis in malaria is caused by antibodies to ScienceDirect
Osmotic Burst Of Blood Cells
Immune Cell Bursting Red Blood Cell – Blood And The Immune System
Malaria Parasites Invading Human Red Blood Cell
White Blood Cell Cytolysis
Hypotonic Hypertonic And Isotonic Solutions – What Happens To A Red Blood Cell?
How The Immune System Actually Works – Immune
Urine Sediment Cell Identification Training Quiz – 1/2
Link to this article: red blood cell bursts cytolysis.
See more articles in the same category here: https://linksofstrathaven.com/how
